At the mid-point of the 2030 target for the Sustainable Development Goals (SDGs), progress towards achieving universal health coverage (UHC) is off track (1). According to the latest data, at least 4.5 billion people — more than half of the world’s population — are not fully covered by essential health services (2). Financial protection is also deteriorating, with two billion people experiencing financial hardship due to out-of-pocket health costs (2). People in vulnerable and marginalized situations, particularly those living in low- and middle-income countries, are affected most severely (3).
UHC2030’s 2024–2027 Strategic Framework describes how UHC2030 operates and adds value, now, on the path towards the next UN high-level meeting on UHC in 2027, and in the last stretch before the 2030 milestone for the SDGs.
The Framework comprises three pathways for change to follow in 2024–2027: advocacy (influencing decisions by political, economic and social institutions to advance UHC), accountability (tracking the implementation of commitments to foster actions, decisions, policies and programmes for UHC), and alignment (convening stakeholders to exchange information and to elevate the importance of alignment with one national plan and of working within national structures to strengthen health systems) (Fig. 1).

A collective, strategic focus on these three pathways can result in the changes we need to see by 2027 and can help countries achieve SDG target 3.8, “achieving universal health coverage” by 2030. This Strategic Framework was developed through an inclusive consultation process involving all UHC2030 constituencies.
UHC2030’s collective efforts on advocacy, accountability and alignment in 2024–2027 can help drive progress to ensure that, by 2030, everyone, everywhere, has access to the full range of quality health services they need, when and where they need them, without financial hardship.
I. UHC2030's vision, mission, key principles and unique value

UHC2030’s vision is a world where all people have access to the full range of quality health services they need, when and where they need them, without financial hardship.
UHC2030’s mission is to accelerate sustainable progress towards UHC, focusing on building equitable and resilient health systems that leave no one behind and that provide the foundation to achieve health security.
To become a partner of UHC2030 (5), organizations must sign the Global compact for progress towards universal health coverage. In doing so, they commit to building and extending equitable, resilient, sustainable health systems, funded primarily by public finance and based on primary health care, to deliver integrated, comprehensive, people-centred, high-quality health services for all.
They also commit to the following key principles (6):
- Leaving no one behind: a commitment to equity, non-discrimination and a rights-based approach;
- Transparency and accountability for results;
- Evidence-based national health strategies and leadership, with government stewardship to ensure the availability, accessibility, acceptability and quality of service delivery;
- Making health systems everybody’s business, with engagement of citizens, communities, civil society and the private sector; and
- International cooperation based on mutual learning among countries, regardless of their development status and progress in achieving and sustaining UHC, and the principles of development effectiveness.
The unique value of UHC2030 is that it is the leading global, multi-stakeholder platform for bringing together diverse voices and perspectives for the common goal of achieving UHC. UHC2030 does so by sustaining political momentum on UHC commitments and by promoting collective action to strengthen health systems.
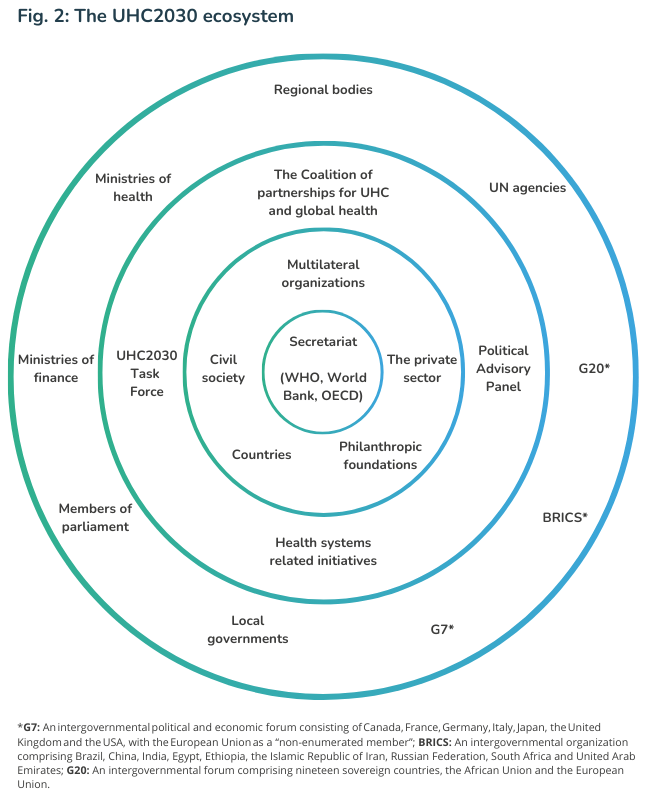
UHC2030 is a global hub for compelling campaigns, coherent communication and tools for tracking implementation of UHC commitments. With its constituency model, UHC2030 can mobilize a wide range of stakeholders (Fig. 2) to ensure that more, better investments for health are made, placing universality, equity, the right to health and health security at the centre of all work.
II. An urgent case for action for UHC

Progress towards UHC is off track. According to the latest data, at least 4.5 billion people — more than half of the world’s population — are not fully covered by essential health services (2). Financial protection is also deteriorating, with 2 billion people experiencing financial hardship due to out-of-pocket health costs (2). People in vulnerable and marginalized situations, including those living in low- and middle-income countries, are most severely affected (3). Furthermore, recent data show that health systems in 136 low- and middle-income countries cannot deliver essential services to women, adolescents and children in need (7).
Progress towards UHC depends on complex, multifaceted factors. Barriers that hinder progress include lack of political will to prioritize people’s health, weak health and information systems, a shortage of health and community health workers, and inadequate health financing. However, reforms to create fiscal space and convert out-of-pocket payments into pooled funding for health are possible and within reach (8). The political attention displayed at the 2023 UN high-level meeting on UHC has yet to be translated into national political priorities, financing, policies and programmes.
UHC has risked falling off agendas since the peak of the COVID-19 pandemic, despite being the key to equitable, resilient health systems that leave no one behind and providing the foundation for health security. Resources may be diverted from national health systems due to increasing competition with other urgent priorities, such as food insecurity, new and expanding large-scale conflicts, and climate change, of which the impact on health and well-being is now widely recognized (9). Without UHC and adequate financing for national health systems, people and communities are more vulnerable to local, regional and global health shocks, placing international stability and prosperity at risk. Disease- and population-specific gains and broader development gains made over the past decades could also be lost. In the context of waning political support, geopolitical tensions, budgetary constraints and other crises, the case for UHC must be made collectively, more clearly and in a way that is compelling for all stakeholders.
The change that UHC2030 aims for by 2027 is the translation, by every country, of the commitments made in the 2023 UN High-level Political Declaration on UHC into laws, budgets, policies and programmes for the achievement of SDG target 3.8 by 2030. Ahead of the next UN high-level meeting on UHC in 2027, UHC2030 will continue to use the Action Agenda from the UHC Movement (10), which provides eight action-oriented policy recommendations and milestones for 2025 to advocate for and strengthen country accountability for progress.
UHC2030’s overarching goal for 2024–2027 is to harness the power of its constituencies and entities to influence the translation of commitments made in the 2023 Political Declaration into action towards the realization of SDG 3.8 by 2030.
Through collective activities and direct action by our constituencies, we can help to ensure that progress on UHC is on track to achieve 2030 targets. Our collective work will support the following UHC dimensions and enablers.
- Universality, equity and the right to health are the starting points of UHC and the key to expanding population coverage. UHC serves all countries and all people, but its implementation must start with the prioritization of the health needs and access of people in vulnerable and marginalized situations, among whom women, adolescents and children are disproportionately represented (7). To ensure that everyone, everywhere has access to health services, efforts must be made to tackle health inequities, barriers to human rights and gender inequality.
- The means to expanding service coverage and achieving UHC and health security is investment in resilient health systems, designed and based on country and population needs (11). The most inclusive, equitable, cost-effective approach is through primary health care (12), to ensure that services are of high quality, safe, comprehensive, integrated, accessible, available and affordable for everyone, everywhere (13). Health systems must be gender-responsive, rights-based, climate-resilient and adaptive. They should also leverage digital opportunities to improve health outcomes.
- Expanding and sustaining financial protection requires adequate public financing and engagement beyond the health sector. It is possible to remove financial barriers and prevent financial hardship by providing access to a core package of health services that are affordable or free-of-charge to people in vulnerable and marginalized situations (2). Securing adequate funding for UHC implementation requires countries to prioritize health, improve the efficiency of health financing, and establish pre-paid, pooled, compulsory contributions (2, 14) through cross-sectoral, multi-stakeholder collaboration and a whole-of-government approach.
- The inclusive governance of health systems through social participation, involving all relevant stakeholders and fostering youth engagement, contributes to building trust. This whole-of-society approach also helps to ensure that health policies and services are responsive, equitable and effective.
III. Pathways for change: advocacy, accountability, alignment
Throughout 2024–2027, UHC2030 will build on its successes to date and focus on three pathways for change: advocacy (influencing decisions by political, economic and social institutions to advance UHC), accountability (tracking the implementation of commitments to foster action, decisions, policies and programmes for UHC) and alignment (convening stakeholders to exchange information and to elevate the importance of alignment with one national plan and of working within national structures to strengthen health systems) (Fig. 3).

IV. Global work and country impact
Rallying around these pathways can further anchor UHC in the global political agenda and ensure that UHC targets become a reality for all people, everywhere by 2030, as committed to by UN Member States in the 2030 Agenda and the SDGs.
Although UHC requires action by many stakeholders, which are beyond the direct scope of UHC2030, a strategic, collective focus on the three pathways for change among UHC2030 constituencies (many of which are engaged at the country level) and global stakeholders can lead to the necessary changes by 2027 and reinvigorate and accelerate progress on UHC by 2030.
Fig. 3 (in section III above) shows how work by UHC2030 constituencies and partners can result in better coordinated activities in 2024–2027 and in strategically effective outputs by 2027.

V. Collective action and targets
Various constituencies and partners will contribute to UHC2030’s collective activities and outputs in 2024–2027 (see Fig. 3 and the Annex). Strategic collaboration among constituencies and partners on the three pathways, the output targets and UHC2030’s collective added value are outlined below. The outcome and impact targets for 2030 will require action by many stakeholders beyond the direct scope of UHC2030’s work, particularly at the country level.
Advocacy

Influencing decisions by political, economic and social institutions to advance UHC
UHC2030 serves as a global hub for compelling campaigns and coherent, evidence-based communication on UHC that places universality, equity, the right to health and health security at the centre. The UHC2030 Secretariat supports all of its constituencies and partners in their advocacy and outreach efforts, prioritizing primary health care, equitable and resilient health systems, financial protection, and inclusive governance for health. All UHC2030 constituencies and partners base their recommendations on evidence and ensure common messaging to advocate for action on UHC at key global events and political processes, including beyond the health sector. Moreover, many UHC2030 constituencies engage at the country level. The value that UHC2030 adds is helping to tailor evidence-based political advocacy and to leverage opportunities for outreach at key global, regional and national events.
Between 2024 and 2027, UHC2030 collectively aims to meet the following targets:
- Target 1: UHC is featured on the agendas of relevant global and regional political events, and all stakeholders are united to support UHC2030 evidence-based advocacy.
- Target 2: UHC2030 advocacy and communication materials are used to inform relevant national political processes
Accountability

Tracking the implementation of commitments to foster action, decisions, policies and programmes for UHC
Using evidence, including the Global Monitoring Report on UHC (2), and consultations with stakeholders, such as through multi-stakeholder reviews, the UHC2030 Secretariat contributes to global UHC accountability by tracking action on commitments (e.g., through the State of UHC Commitment Review (15) and Action Agenda milestones (10)) and stimulating discussion on findings and trends. UHC2030 constituencies use this evidence and the broad range of UHC expertise in UHC2030 constituencies and networks in countries to: mobilize political commitment for UHC; support countries in resolving barriers to progress on UHC; and foster multi-directional accountability for UHC. UHC2030 adds value by providing common, evidence-based tools for tracking and by regularly communicating on the implementation of UHC commitments.
Between 2024 and 2027, UHC2030 collectively aims to meet the following targets:
- Target 1: UHC2030’s tracking tools are used by constituencies and partners to strengthen government accountability for implementing the commitments made at the 2023 UN High-level Meeting on UHC and for translating global commitments into national action.
- Target 2: The evidence provided in UHC2030’s tracking tools is used by UHC2030 constituencies and partners in political outreach and engagement and to support countries in resolving barriers to progress on UHC.
Alignment

Convening stakeholders to exchange information and elevate the importance of alignment with one national plan and of working within national structures to strengthen health systems
By maintaining high visibility with evidence-based, collective communication products and outreach and building on the Lusaka Agenda (16), the UHC2030 Secretariat mobilizes global support for greater alignment of stakeholders and external funding partners with national priorities and for the use of country systems to build equitable, resilient health systems. This includes promoting the engagement of civil society and communities. UHC2030 constituencies share their experience on alignment with national priorities and linking UHC to other priority areas (such as climate change and health emergency prevention, preparedness and response). UHC2030’s added value is the regular convening of stakeholders for global dialogue and exchange on good practices in: (a) alignment with national priorities for health systems strengthening and UHC; and (b) using one national plan and government systems for public financial management to ensure that domestic and external financial resources are invested and used effectively and in a concerted manner. UHC2030 will do so in close coordination with relevant actors and initiatives, including the UHC Partnership, WHO’s largest initiative on UHC and primary health care, which serves as a platform for donors to work together in transforming global commitments to tangible results in countries.
Between 2024 and 2027, UHC2030 collectively aims to meet the following targets:
- Target 1: The importance of aligning work, in particular for international funding, with health systems strengthening and UHC is featured prominently in collective advocacy and on global and regional agendas.
- Target 2: UHC2030 constituencies have taken action to support alignment with one national plan and government systems for public financial management and exchange information on their actions.
VI. UHC2030 constituency activities and outputs
This section outlines the key activities and outputs of UHC2030 constituencies in 2024–2027, as part of their engagement with UHC2030.
Countries
Countries at all income levels can create the conditions in which the right to health is ensured, upheld and respected for everyone and commitments to UHC in the Political Declaration are met. On advocacy, countries will ensure that UHC is high on global and regional agendas by promoting the inclusion of UHC and health systems strengthening in multilateral negotiations. They will also advocate for achieving UHC targets, including prioritizing the health needs and access of people in vulnerable and marginalized situations in their own national institutional processes. Countries will strengthen their accountability and resolve barriers to progress towards UHC by using the State of UHC Commitment reviews (15) and other tracking tools to review progress and by improving reporting in voluntary national reviews on achievement of the SDGs. Building on the Lusaka Agenda (16) and the WHO Fourteenth General Programme of Work, countries will support alignment behind more efficient, effective global funding for health systems strengthening and UHC by promoting coherence on issues such as resource mobilization, project implementation, monitoring and evaluation, and replenishment for global health initiatives.
Multilateral organizations
As entities that work on multisectoral issues that transcend national boundaries and cannot be solved by one country or sector alone, UN agencies will highlight the importance of UHC for broader development and for population- and situation-specific targets. On advocacy, they will make efforts to ensure that UHC is included on agendas for global and regional policy events and processes through their regional and country offices and at headquarters. They will also ensure that UHC2030 materials inform relevant technical meetings and national policies. On accountability, they will support the dissemination of UHC2030 tools and products for tracking implementation, including in forums on subjects other than health. On alignment, they will support the channeling of international funding for health systems strengthening and will contribute to achieving country priorities by developing partnerships and taking country-level coordinated action.
As global financing entities, global health initiatives will ensure that funding is effectively aligned for achieving UHC. On advocacy, they will ensure that UHC is featured on global and regional agendas and that its importance is emphasized in multilateral and national processes. To strengthen countries’ accountability for progress towards UHC, they will provide evidence-based data and share experiences in measuring accountability. On alignment, global health initiatives will also work towards coordinating and aligning their investments in health systems and their overall work on health systems strengthening to build on the Lusaka Agenda.
Civil society organizations
Through the civil society engagement mechanism platform, civil society organizations will work to ensure that UHC policies are inclusive and equitable, and that attention is systematically paid to people in marginalized and vulnerable situations to ensure that no one is left behind. On advocacy, they will ensure that UHC is featured high on agendas by advocating for UHC at key global and regional events and on UHC Day, and they will make the case for UHC before national elections. On accountability, they will help to identify and address challenges, in particular for people left behind, by engaging with communities in need and at risk at country levels. They will hold countries accountable by contributing to the development of the State of UHC Commitment review and by using evidence from this and other reviews. On alignment, they will lobby global actors and engage with parliamentarians to strengthen national priorities for UHC.
Philanthropic foundations
Philanthropic foundations will use their convening power, expertise and funding to advance progress towards UHC. On advocacy, they will persuade the organizers of global and regional events to include UHC on agendas and to share evidence-based messages on UHC. On accountability, they will work to remove barriers to UHC and support strengthening and dissemination of tools for tracking UHC implementation. On alignment, they will ensure that their funding and that of other grantees supports health systems strengthening and UHC.
The private sector
The private sector will provide a collaborative platform for entities interested in fostering dialogue and cooperation on UHC. On advocacy, they will help to raise awareness about the importance of UHC in the global and regional arena by using UHC2030’s evidence-based messages to publish op-eds and engage in UHC-related events. To foster accountability, they will help monitor action on commitments and remove barriers to progress towards UHC, as detailed in the statement on private sector commitments to UHC in 2023 (17). On alignment, they will support health systems strengthening by facilitating collaboration in joint private sector-government events and exchanging best practices, in the spirit of building trust.
References
- SDG target 3.8. Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all. The Global Health Observatory. Geneva: World Health Organization; 2024 (https://www.who.int/data/gho/data/themes/topics/indicator-groups/indicator-group-details/GHO/sdg-target-3.8-achieve-universal-health-coverage-(uhc)-including-financial-risk-protection).
- WHO and the International Bank for Reconstruction and Development. Tracking universal health coverage: 2023 global monitoring report. Geneva: World Health Organization; 2023 (https://www.who.int/publications/i/item/9789240080379).
- United Nations General Assembly. New York: United Nations; 2023.
- Universal health coverage (UHC). Geneva: World Health Organization; 2024 (https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(uhc)).
- UHC2030 partners. Geneva: World Health Organization; 2024 (https://www.uhc2030.org/who-we-are/uhc2030-partners/).
- Global compact. Geneva: World Health Organization; 2024 (https://www.uhc2030.org/what-we-do/improving-collaboration/global-compact/).
- World Health Organization, United Nations Children’s Fund. Protect the promise: 2022 progress report on the every woman every child global strategy for women's, children's and adolescents’ health (2016-2030). Geneva: World Health Organization; 2022 (https://www.who.int/publications/i/item/9789240060104).
- Universal health coverage and health outcomes. Final report. Paris: Organisation for Economic Co-operation and Development; 2016 (https://www.oecd.org/health/health-systems/Universal-Health-Coverage-and-Health-Outcomes-OECD-G7-Health-Ministerial-2016.pdf).
- COP28 UAE declaration on climate and health. Geneva: World Health Organization; 2023 (https://www.who.int/publications/m/item/cop28-uae-declaration-on-climate-and-health).
- Action agenda from the UHC movement. Geneva: World Health Organization; 2023 (https://www.uhc2030.org/un-hlm-2023/action-agenda-from-the-uhc-movement/).
- Ready for the next crisis? Investing in health system resilience (OECD Health Policy Studies). Paris: Organisation for Economic Co-operation and Development; 2023. doi:10.1787/1e53cf80-en.
- Realising the potential of primary health care (OECD Health Policy Studies). Paris: Organisation for Economic Co-operation and Development; 2020. doi:10.1787/a92adee4-en.
- Declaration of Astana. Geneva: World Health Organization; 2018 (https://www.who.int/publications/i/item/WHO-HIS-SDS-2018.61).
- Fiscal sustainability of health systems: How to finance more resilient health systems when money is tight? Paris: Organisation for Economic Co-operation and Development; 2024. doi:10.1787/880f3195-en.
- State of UHC commitment. Geneva: World Health Organization; 2023 (https://www.uhc2030.org/what-we-do/voices/state-of-uhc-commitment/).
- Future of Global Health Initiatives. Final outputs. London: Wellcome Trust; 2023 (https://futureofghis.org/final-outputs/).
- Private sector commitments to universal health coverage. UHC2030 private sector constituency 2023 statement Geneva: World Health Organization; 2023.
Photo credits: Page 2 - Tbel Abuseridze on Unsplash; Page 6 - ©WHO / Blink Media - Lisette Poole; Page 7 - ©WHO / Ismail Taxta; Page 10 - ©WHO / Ploy Phutpheng; Page 11 - ©WHO / NOOR / Sebastian Liste; Page 12 - WHO / Blink Media - Gilliane Soupe; Page 13 - Marco Oriolesi on Unsplash
Resources
- PDF version of the 2024-2027 Strategic Framework: English French Spanish
- Co-chair statement to launch the 2024-2027 Strategic Framework: The imperative case for universal health coverage (UHC): Fostering the translation of UHC commitments into action
- About UHC2030
- Action Agenda from the UHC movement
- 2023 Political Declaration on universal health coverage
- State of UHC Commitment
- Tracking universal health coverage: 2023 global monitoring report
- UHC2030 newsletters